About the Procedure
Patient Information Guide
Understanding Deep Venous Obstruction
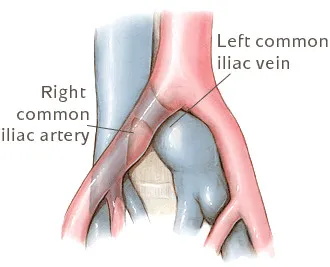
Deep venous obstruction occurs when blood flow in the veins of your pelvic area or lower abdomen (iliofemoral veins) is reduced or blocked. While arteries carry oxygen-rich blood from the heart to the body, veins return blood back to the heart to be reoxygenated. When your leg veins cannot return enough blood, it may lead to leg swelling, pain, skin changes, or ulcers.
Pelvic Venous Disorder
Pelvic venous disorder (previously known as Pelvic Venous Congestion) - A vascular disorder that results in abnormally dilated veins in the pelvis. It can be confused with hormonal abnormalities or dysfunction, ovarian cysts, irritable bowel syndrome, painful bladder, other gynecological factors and psychological factors.
Prevalence of pelvic venous disorder
Impacts 15% of females aged 18-65 in the US
Accounts for 40% of outpatient gynecologic visits & laparoscopies
30-40% of chronic pelvic pain cases are associated with pelvic venous disorder
Most common in women who have more than one childbirth
Signs and Symptoms
The main signs are pelvic pain/pressure for more than six months, pain during and after intercourse, and an unusually high degree of discomfort during menstruation.
Feelings of fullness and swelling the vaginal, labia, or perineal regions
Aching pain in the lower back and pelvis
Vaginal or vulvar varicose veins
Varicose veins of the upper thigh, top of the inner thighs, or back of the thighs
Irritable bladder (sometimes leading to stress incontinence)
Risk Factors
Most often occurs in women who have had previous pregnancies but can also occur in some women with no pregnancy history
Age
Family history
Obesity
Hysterectomies and other pelvic or abdominal surgeries
Iliac vein recanalization and stenting accelerates healing of venous leg ulcers associated with severe venous outflow obstruction
Iliac vein compression is highly comorbid in patients with chronic venous leg ulcers and is a barrier to healing
Healing time is improved and ulcer-free time increased after venous intervention with stenting to eliminate compression.
What Is the Venous Self-Expanding Stent System?
The venous stent system includes both a stent and a delivery system:
The stent is a flexible, self-expandable mesh tube made of nitinol (nickel and titanium).
The delivery system is a long, thin device used to position and deploy the stent in the affected vein.
Once placed, the stent opens the narrowed or blocked vein, supports the vein wall, and allows blood to flow freely toward the heart. The stent remains in place permanently to keep the vein open and restore function.
Benefits of the Venous Stent
The primary benefit of venous stenting is to open compressed or obstructed veins and restore blood flow. This procedure may improve symptoms of venous disease, including:
Leg pain and discomfort
Swelling
Skin changes
Venous ulcers
By improving circulation, stenting can also enhance your overall quality of life.
What to Expect
Before
Your doctor will review your medical history, current medications, and any past treatments.
A physical exam may be done to check for swelling or skin changes.
Imaging tests such as IVUS, venogram, CT, or MR venography may be used to evaluate your veins.
You may receive instructions on eating, drinking, or adjusting medications before the procedure.
During
You will receive anesthesia to minimize discomfort.
A small needle is inserted in the leg, neck, or arm to access the obstructed vein.
A balloon may be used to help open the vein before placing the stent.
The stent self-expands to hold the vein open. Sometimes multiple stents are placed.
Your doctor may use IVUS or venogram to confirm the stent is properly positioned.
After
Most patients can return home the same day.
Your doctor may perform an ultrasound to confirm vein function.
Follow-up visits and medications may be prescribed.
Staying active and living a healthy lifestyle are important for long-term vein health.
Ready to get started?
